Feeling lightheaded or fainting can be a frightening experience, especially when it happens unexpectedly. Vasovagal syncope, a condition characterized by sudden drops in blood pressure and heart rate, is a common cause of these episodes. For those living with this condition, managing daily activities can pose unique challenges. Understanding the triggers and adopting effective strategies to manage symptoms is key to improving quality of life. In this post, we’ll delve into practical tips and insights on living with vasovagal syncope, helping you regain confidence and control over your day-to-day life.
What is Vasovagal Syncope?
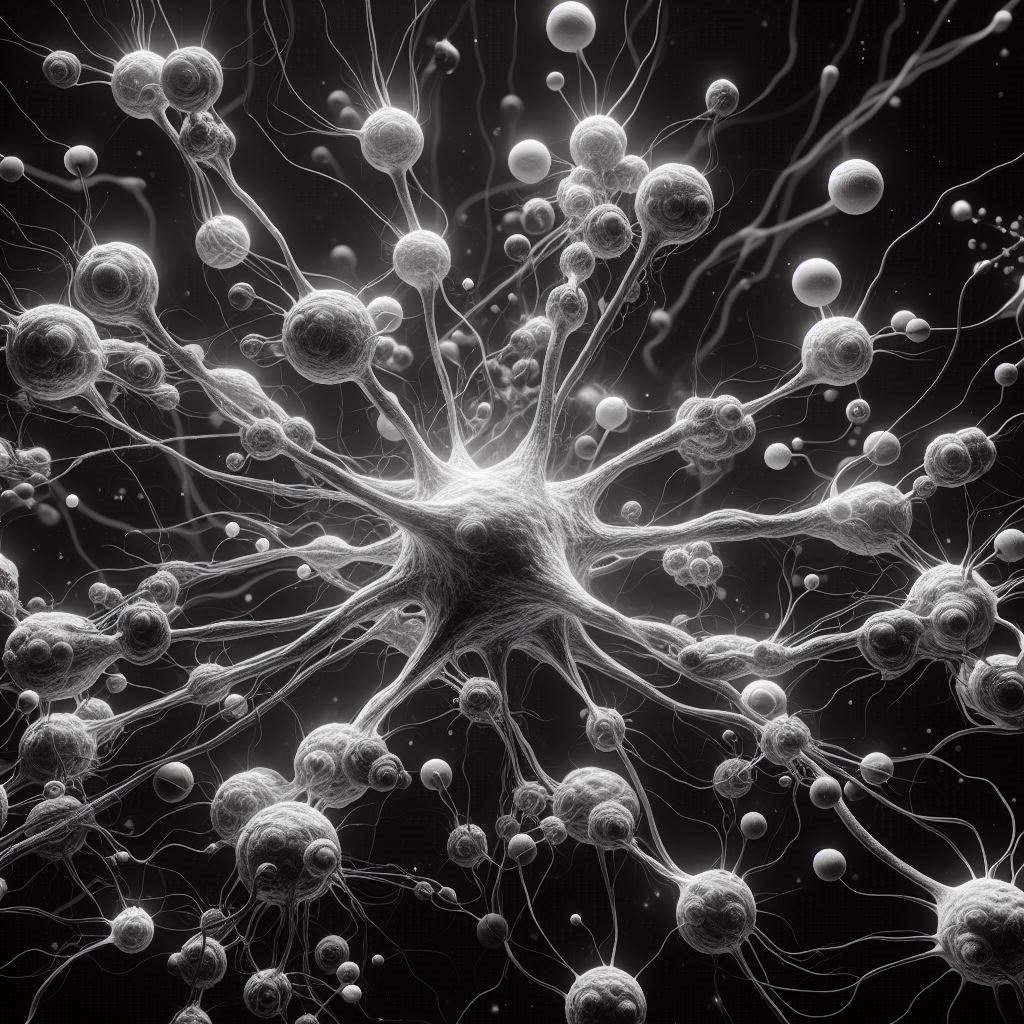
Vasovagal syncope is a condition characterized by a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. This phenomenon occurs due to a malfunction in the body’s normal response mechanisms, specifically the autonomic nervous system.
Definition and Causes:
The mechanism behind vasovagal syncope involves a sudden dilation of blood vessels and a decrease in heart rate, resulting in blood pooling in the legs and reducing blood flow to the brain. Common triggers of vasovagal syncope include emotional stress, dehydration, standing for long periods, pain, and certain medical procedures. Understanding these triggers is crucial in managing the condition and preventing episodes.
Symptoms:
Recognizing the signs that precede a vasovagal episode is essential for early intervention. Symptoms may include dizziness, lightheadedness, nausea, sweating, blurred vision, and a sudden feeling of warmth. Some individuals may also experience a brief loss of consciousness, commonly referred to as fainting or passing out.
Diagnosis:
Healthcare professionals diagnose vasovagal syncope through a combination of medical history evaluation, physical examinations, and specific tests like tilt table tests. During a tilt table test, the patient lies flat on a table that is then tilted to simulate an upright position. Monitoring the individual’s response to this change helps in confirming the diagnosis and understanding the underlying mechanisms triggering vasovagal episodes.
For more in-depth information on vasovagal syncope, you can refer to reputable sources such as the Cleveland Clinic and Cedars-Sinai.
Living with Vasovagal Syncope
Living with vasovagal syncope can present challenges, but there are strategies that can help manage symptoms, prepare for emergencies, and establish strong support systems to navigate this condition effectively.
Managing Symptoms
When living with vasovagal syncope, it’s essential to incorporate lifestyle adjustments to alleviate symptoms. Here are some practical tips to consider:
- Stay Hydrated: Dehydration can exacerbate symptoms of vasovagal syncope. Ensure you drink an adequate amount of water throughout the day to maintain hydration levels.
- Avoid Triggers: Identify specific triggers that may lead to fainting episodes and try to avoid them. Common triggers include prolonged standing, heat exposure, and stressful situations.
- Use Compression Stockings: Wearing compression stockings can help improve blood circulation and prevent blood pooling in the legs, reducing the risk of fainting.
Emergency Preparedness
It’s crucial to be prepared for fainting episodes that may occur with vasovagal syncope. Here are some steps to follow during an episode:
- Lie Down: If you feel like you are about to faint, lie down on your back to prevent injury from falling.
- Elevate Legs: Elevating your legs above the level of your heart can help improve blood flow to your brain and vital organs, potentially reducing the intensity of the fainting episode.
Support Systems
Building a robust support network is integral when living with vasovagal syncope. Consider the following support systems to aid in coping with this condition:
- Friends and Family: Inform your close circle of friends and family about your condition so they can provide assistance or support when needed.
- Healthcare Providers: Establish open communication with healthcare professionals who can offer medical guidance, treatment options, and monitor your condition closely.
By incorporating these lifestyle adjustments, emergency preparedness measures, and a reliable support system, individuals living with vasovagal syncope can enhance their quality of life and effectively manage the challenges associated with this condition.
For more information and advice on living with vasovagal syncope, you can refer to resources such as Advice for patients who tend to faint (Vasovagal Syncope) and Vasovagal Syncope: Symptoms, Causes and Treatment.
Treatment Options
Living with vasovagal syncope can be challenging, but there are various treatment options available to manage the condition effectively. These treatments aim to reduce the frequency and severity of vasovagal syncope episodes, improving the quality of life for individuals dealing with this condition.
Medical Interventions
Medical interventions play a crucial role in managing severe cases of vasovagal syncope. Here are some common approaches:
- Medications: Medications such as fludrocortisone acetate, typically used to treat low blood pressure, may be prescribed to help prevent vasovagal syncope episodes. Beta-blockers and other drugs have also been tested to manage symptoms effectively (source).
- Pacemakers: In cases where vasovagal syncope is associated with a cardioinhibitory response, pacemakers can be a potential treatment option. Pacemakers help regulate the heart rate and rhythm, reducing the risk of syncope episodes (source).
Therapies and Techniques
Complementary therapies and techniques can be beneficial in managing vasovagal syncope symptoms and improving overall well-being. Consider the following approaches:
- Cognitive Behavioral Therapy (CBT): CBT has shown effectiveness in individuals with challenging-to-manage vasovagal syncope. This therapy focuses on helping individuals understand and cope with triggers that may lead to syncope episodes, potentially reducing their frequency (source).
- Stress Management: Learning stress management techniques can help individuals with vasovagal syncope better control their body’s responses to stressors, potentially decreasing the likelihood of syncope episodes. Techniques such as deep breathing, mindfulness, and relaxation exercises can be beneficial.
By exploring a combination of medical interventions and complementary therapies, individuals living with vasovagal syncope can work towards managing their condition effectively and improving their quality of life. Seeking guidance from healthcare professionals and exploring personalized treatment plans tailored to individual needs are crucial steps in effectively managing vasovagal syncope.
Coping Strategies
Living with vasovagal syncope can bring about various challenges that go beyond the physical symptoms. The psychological impact of dealing with this condition is significant, often leading to feelings of anxiety and a constant fear of fainting in public settings. These emotional struggles can be overwhelming and affect one’s quality of life.
Psychological Impact
The psychological effects of vasovagal syncope can be profound. Individuals may experience heightened anxiety due to the unpredictability of fainting episodes. The fear of fainting in public places can lead to social withdrawal and avoidance of certain activities. It’s essential to address these emotional aspects and seek support to cope effectively.
To manage the psychological impact of vasovagal syncope, consider the following strategies:
- Seeking Counseling: Talking to a therapist or counselor can help you process your emotions and develop coping mechanisms.
- Joining Support Groups: Connecting with others who also live with vasovagal syncope can provide a sense of community and understanding.
- Practicing Mindfulness: Engaging in mindfulness techniques like deep breathing and meditation can help reduce anxiety levels.
- Educating Yourself: Understanding your condition better can empower you to navigate challenges more effectively.
Self-Care Practices
In addition to addressing the psychological effects, incorporating self-care practices into your daily routine can significantly improve your overall well-being when living with vasovagal syncope. These practices aim to enhance both physical and emotional resilience.
Consider the following self-care practices to manage vasovagal syncope:
- Mindfulness Techniques: Practicing mindfulness can help you stay present and reduce stress levels. Consider mindfulness apps or guided meditation sessions.
- Relaxation Techniques: Engage in activities that promote relaxation, such as yoga or tai chi, to alleviate tension and promote a sense of calm.
- Regular Exercise: Incorporating regular physical activity into your routine can improve cardiovascular health and boost overall well-being. Consult your healthcare provider for exercise recommendations tailored to your needs.
- Healthy Sleep Habits: Prioritize adequate sleep to support your body’s recovery and resilience. Establish a bedtime routine and create a restful sleep environment.
By implementing these coping strategies and self-care practices, you can enhance your quality of life while managing vasovagal syncope more effectively. Remember to prioritize your mental and physical well-being, and seek professional guidance when needed to navigate the challenges associated with this condition.
Key Takeaways
Living with vasovagal syncope can present unique challenges but understanding key takeaways can aid in managing this condition effectively.
Stay Hydrated and Maintain a Balanced Diet
Ensuring proper hydration and a balanced diet can help regulate blood pressure and reduce the likelihood of vasovagal syncope episodes. Consuming adequate fluids and nutritious meals can contribute to overall well-being and symptom management.
Recognize Triggers and Learn Relaxation Techniques
Identifying triggers such as stress, heat, or prolonged standing can assist in preventing episodes. Practicing relaxation techniques like deep breathing exercises or mindfulness can help manage anxiety and potentially mitigate the impact of triggers on vasovagal syncope.
Seek Medical Guidance and Treatment Options
Consulting healthcare professionals for a proper diagnosis and personalized treatment plan is crucial for individuals living with vasovagal syncope. Understanding available treatment options, including lifestyle modifications or medications, can improve quality of life and minimize symptom severity.
Establish Support Systems and Educate Others
Building a support network of family and friends who are aware of your condition can offer assistance during episodes. Educating loved ones about vasovagal syncope, its symptoms, and appropriate responses can promote a safe environment and prompt care when needed.
Maintain Regular Follow-ups and Track Symptoms
Regular follow-up appointments with healthcare providers can track progress, adjust treatment plans, and address any concerns. Keeping a symptom journal to record triggers, frequency of episodes, and any notable changes can provide valuable insights for better symptom management and communication with medical professionals.
For more detailed information on vasovagal syncope, you can refer to the Cleveland Clinic’s guide on symptoms, causes, and treatments or explore resources from the NHS Lanarkshire for additional advice and strategies.
Vasovagal Syncope: Living with Vasovagal Syncope Management
Managing vasovagal syncope is key to improving your quality of life and minimizing the impact of fainting episodes. Here’s a closer look at proactive symptom management strategies and essential steps to navigate life with vasovagal syncope.
Understanding Proactive Management
Proactive management involves a combination of lifestyle changes, non-pharmacological treatments, and potentially medication under the guidance of a healthcare professional. Lifestyle adjustments such as staying hydrated, avoiding triggers, and increasing salt intake can help prevent syncope episodes.
Importance of Treatment Pathways
Non-pharmacological treatment options serve as a foundational approach in managing vasovagal syncope. These strategies, including physical counterpressure maneuvers and addressing underlying factors like anxiety, play a crucial role in symptom management.
Hope Through Effective Symptom Management
While living with vasovagal syncope can present challenges, proactive symptom management offers hope for improved daily functioning and reduced episodes of syncope. By working closely with healthcare providers to develop a personalized management plan, individuals can regain a sense of control over their condition.
Don’t hesitate to explore various management approaches and seek support to enhance your quality of life while living with vasovagal syncope.
For more information on vasovagal syncope management, you can refer to resources such as articles on management and therapy of vasovagal syncope and the Oxford Academic’s insights on the management of vasovagal syncope.